The Dual Diagnosis Approach: Treating Co-Occurring Mental Health and Substance Use Disorders Together

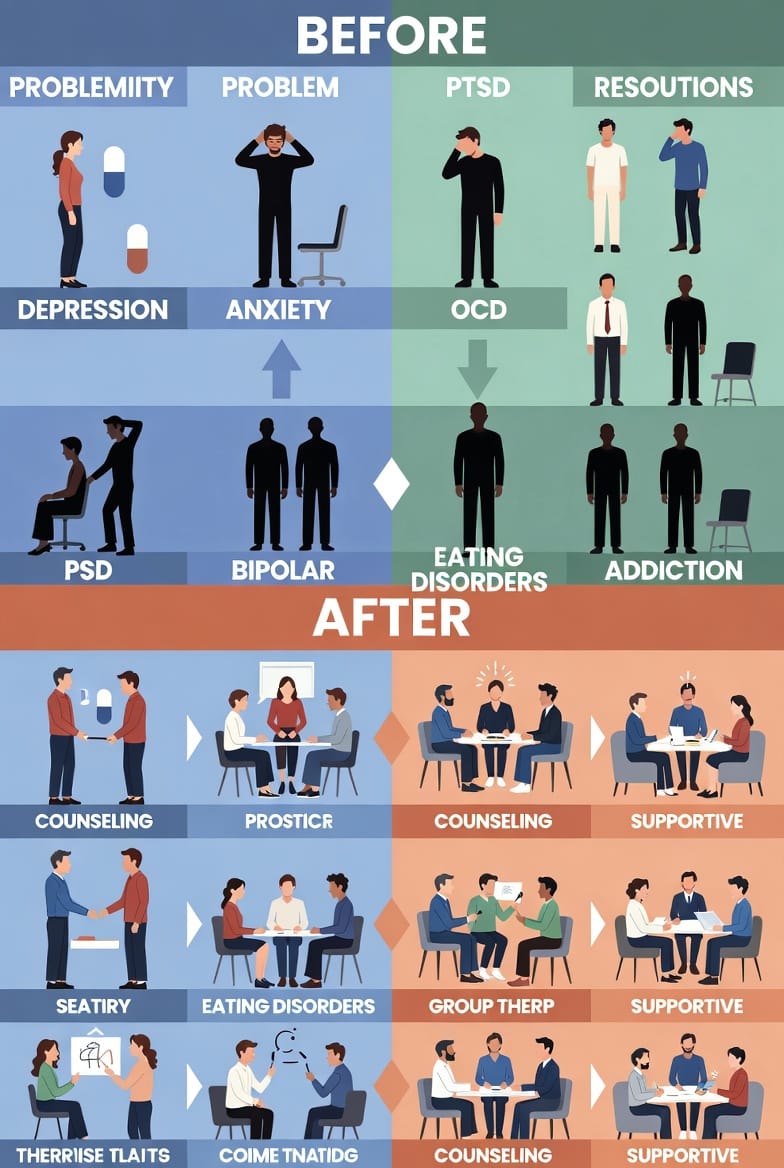
In the realm of addiction recovery, dual diagnosis stands as a critical concept that recognizes the intricate interplay between mental health disorders and substance use disorders. Far too often, individuals facing addiction are also grappling with underlying conditions such as depression, anxiety, or PTSD, creating a complex web of challenges that demand a comprehensive response. This article explores the nuances of these concurrent disorders, why isolated treatment approaches frequently fall short, and how integrated dual diagnosis programs offer a pathway to sustainable healing. By addressing both aspects simultaneously, these programs foster lasting recovery, empowering individuals to reclaim their lives with confidence.
Break the Cycle of Relapse – Call for Integrated Care
Understanding Dual Diagnosis: The Complexity of Concurrent Disorders
Dual diagnosis, also known as co-occurring disorders, refers to the simultaneous presence of a mental health condition and a substance use disorder. This isn't a rare occurrence; in fact, statistics from leading health organizations indicate that nearly half of those with a substance use disorder also experience a mental health issue, and vice versa. The complexity arises because these conditions often feed into one another, forming a vicious cycle that's difficult to break without targeted intervention.
Consider the brain's role in this dynamic. Substance abuse can alter neural pathways, exacerbating symptoms of mental illness, while untreated emotional distress may drive someone to self-medicate with drugs or alcohol. For instance, a person with anxiety disorder might turn to alcohol for temporary relief, only to find that chronic use deepens their anxiety over time. This bidirectional relationship underscores why concurrent disorders are not just additive but multiplicative in their impact.
- Prevalence: Up to 50% of individuals seeking treatment for addiction have a co-occurring mental health diagnosis.
- Common Triggers: Trauma, genetics, environmental stressors, and neurochemical imbalances often contribute to the onset.
- Diagnostic Challenges: Symptoms can overlap, making accurate identification essential for effective care.
Rest assured, recognizing this complexity is the first step toward empowerment. With the right approach, even the most entangled cases can be unraveled, leading to profound transformation.
The Pitfalls of Sequential or Isolated Treatment
Treating addiction in isolation—without addressing underlying mental health conditions—is akin to patching a leak without fixing the pipe. This fragmented method often leads to relapse, as the root causes remain unaddressed. Research consistently shows that individuals who receive care for only one disorder are at a significantly higher risk of returning to substance use.
Why does this happen? When depression or anxiety persists untreated, the emotional pain can become overwhelming, prompting a return to old coping mechanisms. Similarly, PTSD survivors might experience flashbacks or hypervigilance that drive them back to substances for numbness. Without simultaneous care, the untreated condition acts as a hidden trigger, undermining progress.
- Relapse Rates: Studies reveal that up to 60% of those treated for addiction alone relapse within the first year if mental health issues are ignored.
- Cycle of Frustration: Patients may feel defeated, leading to lower engagement in future treatment attempts.
- Long-Term Consequences: Untreated co-occurring disorders can result in worsened physical health, strained relationships, and increased societal costs.
The good news is that this doesn't have to be the outcome. By shifting to an integrated model, we can break this cycle and build resilience from the ground up.

Why Integrated Dual Diagnosis Programs Succeed
Integrated dual diagnosis programs represent a paradigm shift, providing simultaneous, coordinated care for both mental health and substance use disorders. In these programs, a multidisciplinary team—including psychiatrists, therapists, addiction counselors, and support staff—works collaboratively to create personalized treatment plans. This holistic approach ensures that neither condition is sidelined, promoting synergy in healing.
At the core is evidence-based therapy, tailored to the individual's needs. For example, cognitive-behavioral therapy (CBT) might be used to reframe negative thought patterns contributing to both depression and addiction, while medication-assisted treatment (MAT) stabilizes brain chemistry. Group sessions foster community, reducing isolation, and family involvement strengthens support networks.
- Coordinated Assessments: Initial evaluations screen for both disorders, ensuring no aspect is overlooked.
- Tailored Interventions: Therapies like dialectical behavior therapy (DBT) address emotional regulation, complementing detox and relapse prevention.
- Holistic Support: Nutrition, exercise, and mindfulness practices enhance overall well-being.
Authoritative studies from institutions like the Substance Abuse and Mental Health Services Administration (SAMHSA) affirm that integrated care yields higher retention rates and better outcomes. Patients report feeling truly seen and supported, which builds trust and motivation.
Common Co-Occurring Disorders and Tandem Treatments
Certain mental health conditions frequently co-occur with substance use disorders, each requiring a nuanced, tandem approach. Here's a closer look at some prevalent pairings and how integrated programs address them:
- Depression and Alcohol Use Disorder: Depression's low mood can lead to alcohol as a depressant "escape." Tandem treatment combines antidepressants with motivational interviewing to build coping skills and reduce cravings.
- Anxiety and Opioid Addiction: Heightened worry often fuels opioid misuse for calm. Integrated care uses exposure therapy alongside naloxone training and gradual tapering.
- PTSD and Cocaine Dependence: Trauma flashbacks may trigger stimulant use for alertness. Programs pair trauma-focused therapy like EMDR with behavioral interventions to manage triggers.
- Bipolar Disorder and Polysubstance Abuse: Mood swings can drive erratic substance use. Stabilizing medications are synced with addiction counseling to prevent manic episodes.
- Schizophrenia and Cannabis Use Disorder: Hallucinations might prompt self-medication. Antipsychotics are coordinated with psychoeducation on substance risks.
By treating these in tandem, programs mitigate risks and amplify recovery potential, turning vulnerabilities into strengths.
The Benefits of Treating the Whole Person
Embracing a dual diagnosis approach yields multifaceted benefits, extending beyond symptom relief to profound life changes. Participants often experience improved emotional stability, stronger relationships, and enhanced daily functioning. Relapse rates drop significantly—sometimes by as much as 50%—as individuals gain tools to navigate life's stressors without substances.
Moreover, this method promotes self-awareness and empowerment. Through education on the interplay of disorders, patients learn to recognize early warning signs, fostering proactive management. Long-term, it reduces healthcare burdens by preventing repeated hospitalizations or crises.
- Emotional Resilience: Better mood regulation leads to sustained sobriety.
- Social Reintegration: Improved interpersonal skills rebuild family and community ties.
- Physical Health Gains: Addressing both disorders often improves sleep, nutrition, and immunity.
In essence, integrated care honors the whole person, acknowledging that true recovery encompasses mind, body, and spirit.
Real-World Impact and Pathways Forward
Countless individuals have transformed their lives through dual diagnosis programs. Take, for example, a veteran battling PTSD and alcohol dependence: Isolated treatment for addiction led to repeated relapses, but an integrated program combining therapy and peer support groups provided the breakthrough needed for sobriety and peace.
Such stories highlight the program's efficacy. If you're navigating similar challenges, know that help is available, and recovery is achievable. Professional guidance ensures a safe, structured journey.
Embracing Lasting Recovery
Treating the whole person is key to lasting recovery. By addressing co-occurring mental health and substance use disorders together, integrated dual diagnosis programs offer hope and healing where fragmented approaches fail. If you or a loved one is ready to take this step, reach out today.
Your Path to True Recovery Starts Here – Call Now